Research suggests that risk of infection may be greatest in the pre-symptomatic period, so having an early identification system in place is critical for mitigating spread.
Key points:
- Data suggests asymptomatic (no symptoms at all) spread carries a low risk
- Presymptomatic viral contagion, however, is highly linked to Covid spread
- Temperature elevation may be one of the earliest signs of presymptomatic risk
- Contagion risk may be highest 1 day before outward symptoms appear
- Infection control systems should center around baseline temperature monitoring to identify early presymptomatic signs
- Employee vaccinations should be encouraged and tracked, but a symptom and temperature screening should take place regardless of vaccination status
For workplaces looking to preserve health and wellness among employees, a contagious illness prevention strategy that works to stop outbreaks before they begin may be key. Research suggests that true asymptomatic infection spread is rare, with the risk of presymptomatic spread being much higher.
Understanding the difference between asymptomatic vs. presymptomatic spread, how it drives infection spread, and what workplaces can do to identify early symptoms in order to preserve and promote health in the workplace are all critical in any infection control policy.
Presymptomatic infection spread
From the pandemic’s beginnings, health officials have warned that Covid-19 was contagious in ways that many viruses are not, simply because it could be spread at higher rates before a person even realized they were sick. This, clearly, makes infection control more challenging. However, what the data has seemed to find is that it’s actually more presymptomatic spread that drives infection spread, not necessarily completely asymptomatic spread.
For instance, research out of France found that in older patients with Covid-19 infection, peak viral load occurred one full day before symptoms even appeared. That means that the research suggests that patients who are infected with Covid-19 are actually the most contagious a full day before they show any noticeable outward symptoms, like cough or a sore throat.
The research lines up with advice from leading health organizations, who have noted that presymptomatic spread of Covid-19 occurs and can lead to outbreaks. For instance, the CDC cited a study out of Singapore that found at least 7 cases out of 243 that were found to be linked to presymptomatic spread.
The CDC also noted a similar study out of Germany that found that while completely asymptomatic spread did not account for any identified Covid cases, presymptomatic spread certainly did. “In this cluster of Covid-19 cases, little to no transmission occurred from asymptomatic case-patients. Presymptomatic transmission was more frequent than symptomatic transmission,” the study concluded.
Asymptomatic vs. presymptomatic
While the above research points to the relevance of presymptomatic spread, it is important to define the difference between asymptomatic vs. presymptomatic. Asymptomatic means the complete absence of any symptoms at all while still being actively infected. An asymptomatic person will be actively infected with the pathogen, but never present any outward signs of being infected throughout the entire course of the infection.
Presymptomatic, on the other hand, describes the period of time before outward or easily identifiable symptoms of the infection become apparent. The infected individual will have the virus or other pathogen present in their body, but have a period of a day or several days before symptoms become apparent. Then, symptoms will appear and persist throughout the course of the infection.
It is thought that while it is possible for asymptomatic individuals to spread an infection, that they may be less likely to spread the infection––the theories behind this vary. It could be that the asymptomatic person has lower viral loads, thus having less physical amounts of the virus to spread. Or, they may have less opportunities to spread the virus in the absence of viral-shedding measures, such as coughing, sneezing, or blowing their nose.
A 2021 analytic model of asymptomatic, presymptomatic, and symptomatic spread found that over half of cases of Covid transmission could be transmitted by asymptomatic individuals. However, the model classified “asymptomatic” as an umbrella category that included both presymptomatic people and those who would go on to develop symptoms.
The difference between asymptomatic and presymptomatic, however, is an important one. And in taking a closer look at the model, it detailed that when you break it down between the two, the majority of spread actually occurred with presymptomatic individuals––35% of the Covid cases were transmitted from presymptomatic individuals, while only 24% were spread from completely asymptomatic people who would never develop symptoms of any kind.
Another systematic review of 94 studies, PLOS One Medicine concluded that based on symptom and testing analysis, a higher proportion of SARS-CoV-2 infections resulted from transmission from presymptomatic individuals than from asymptomatic individuals.
Although the review had some limitations––such as the possibility of inaccurate negative tests––the data still showed that overall, only about 20 percent of people who presented asymptomatically with a Covid-19 infection remained that way throughout the infection.
And while there may always be some realm of debate on the danger of asymptomatic spread, the fact remains that the data shows that presymptomatic people are far more likely to spread the virus than asymptomatic people.
Identifying presymptomatic individuals
With the prospect of understanding that viral kinetics points to a higher likelihood of presymptomatic spread over asymptomatic spread, the challenge to workplaces then becomes identifying those presymptomatic cases that could present a risk of infection spread.
If someone doesn’t have any symptoms yet, how is it possible to identify them as an infection risk?
The answer may lie in taking a closer look at what it means to be presymptomatic. On an outwardly clinical scale, there may be some gray area that exists in the space between presymptomatic and asymptomatic. If data modeling and research analysis relies on health questionnaires and collected or self-reported symptoms, it is entirely possible that those who fall under the category of “presymptomatic” actually do display very subtle, early signs of infection that are simply overlooked.
For instance, it could be a morning that someone woke up feeling a little more fatigued than normal, but chalked it up to not sleeping well the night before. Or maybe it was that slight chill they felt when they went about their routine, but shook off by adding another sweater. Or still yet, maybe it was a slight tickle in their throat that went away after they added a spoonful of honey to their morning cup of tea.
When relying on solely self-reported symptom identification, human error does have the potential to be high. It’s easy to brush aside subtle symptoms or not realize the outward signs that an infection is brewing internally.
But what if there was a way to identify even subtle, presymptomatic signs that an infection risk is present? What if there was a way to help an individual recognize their own symptoms before they even realized the infection was active, prioritizing health preservation for not just the individual, but also the entire workplace as well?
With Wello, there may very well be a way.
Temperature elevation as an early sign of presymptomatic infection
In looking at the issue of how to identify presymptomatic individuals, some research has suggested that temperature elevation may be present before other symptoms even become apparent. This has huge implications for workplaces looking for an effective strategy to mitigate risk.
For instance, according to one study in medRxiv, even slight temperature elevations can be an early indicator of infection. The retrospective cohort study by researchers used electronic health records data from 6,176 residents in 133 nursing homes across the United States to compare Covid-19 cases with recorded temperature readings.
They found that a change from baseline temperature of >0.4C preempted 47% of the SARS-CoV-2 positive nursing home residents’ infections and helped detect the cases 42.2 hours earlier than those who were not screened for temperature. It’s worth noting that older individuals have a lower average body temperature, so when you take these findings and apply them to a general population, chances are the effects would be even more pronounced.
Critically, the effectiveness of early detection of the cases relied on an on-file record of the baseline temperature, as well as the ability to take several readings to calculate a temperature range.
Additionally, the authors of the study mentioned how using automated technology that can track baseline temperatures and detect elevations from the baseline could help identify when testing is needed–potentially even sooner than an individual realizes they are sick and takes voluntary steps for testing.
Infection control strategies in the workplace
As mentioned, the concept of a method of clearly establishing baseline temperatures for all employees, along with ongoing monitoring that would allow for the early identification of any rise above baseline is critical for a workplace looking to establish an active health preservation model.
Unlike a strategy that simply relies on infection control measures during an active outbreak, establishing an early-on model of health preservation allows for a non-invasive strategy that could both prevent an outbreak in the first place and help stop its spread when infection does occur.
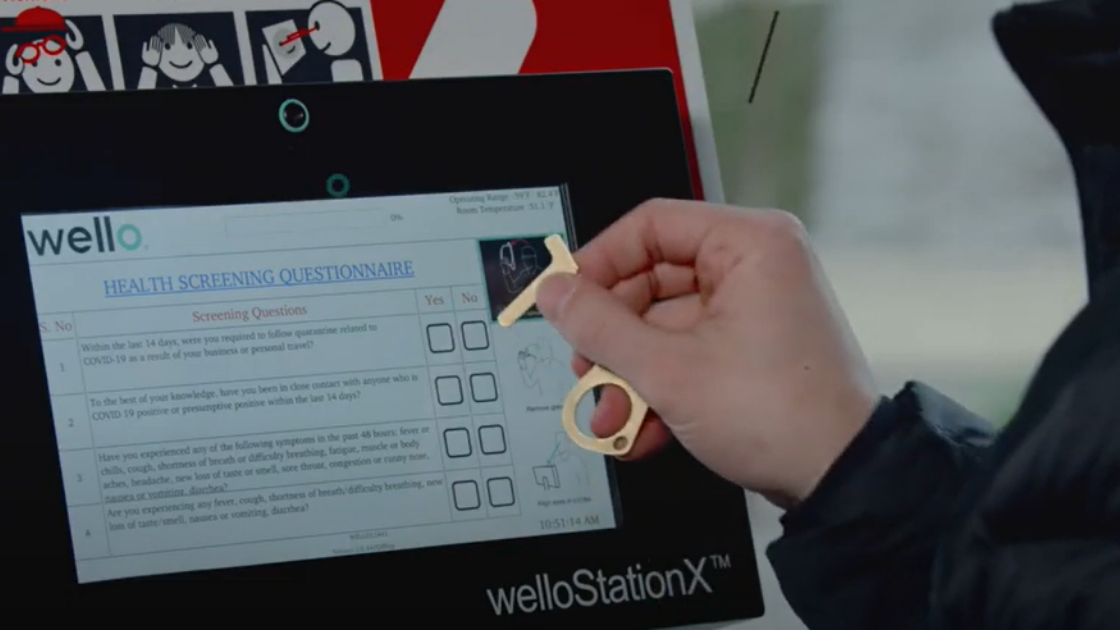
For instance, using an automated health screening technology like welloStationX can help detect potential infections and support testing decisions by respecting and interpreting individual data. The truth is, while an elevated temperature is an early sign of an infection, the degree of elevation varies in everyone––what constitutes a temperature elevation for one person may not translate to an elevation for another, so establishing a baseline temperature (Wello suggests 99.5 degrees Fahrenheit) and logging temperatures over time to analyze trends and detect when a change is found is critical.
Once a change in temperature has been detected based on an individual’s own health data trends, testing may be suggested and appropriate next steps can be determined.
And the result? A safer, healthier and more efficient workplace for everyone.
As it becomes more apparent that “ground zero” with Covid will never become a reality, it is important for workplaces to start to consider and establish future infection control and mitigation strategies that can be used for both Covid and other pathogens. While vaccinations are highly effective at preventing severe disease, the emergence of new variants like Omicron has made it clear that vaccinated individuals can still contract and spread Covid-19. Thus, simply mandating vaccinations and stopping other contagious illness prevention measures leaves businesses at risk of outbreaks.
Even early on in the start of the pandemic, the World Health Organization noted that asymptomatic spread of the virus was rare and that outbreak mitigation strategies should center around identifying symptoms in those who were infected. Now, with more circulating variant strains and different patient populations, it may be helpful for workplaces to implement early symptom detection resources that could help identify possible sources of infection and promote a culture of health and wellness in the workplace.